Postural Orthostatic Tachycardia Syndrome (POTS)
Condition that affects an individual’s blood flow and is more prevalent in women/PWUs.
Postural Orthostatic Tachycardia Syndrome or POTS is a condition that affects an individual’s blood flow. The condition involves the autonomic nervous system which unconsciously controls and regulates certain bodily functions as well as the sympathetic nervous system, the mechanism in charge of our body’s automatic response to stressful events (fight-or-flight response).
It can be difficult to diagnose POTS because it incurs a wide range of symptoms that vary greatly between individuals. In addition to this, POTS can also be hard to diagnose because it may have overlapping symptoms with other illnesses such as anxiety. It may take years or months before a patient is diagnosed with POTS.
SYMPTOMS
Symptoms of POTS can detract from a patient’s quality of life if left untreated. Symptoms of POTS are caused by:
- Lower amount of blood in circulation.
- Excessive pooling of blood when standing upright.
- High levels of certain hormones, (such as epinephrine).
From a horizontal position (i.e., lying down), adults with POTS will have a heart rate that increases by at least 30 bpm when they stand. Comparatively, an adolescent with POTS will have a heart rate that increases by 40 bpm as they stand from a horizontal position. POTS is also characterized by the development of unpleasant symptoms when standing. Although not all patients experience these symptoms, they may experience two or more of the symptoms listed below:
The most common POTS symptoms are:
-
Lightheadedness
-
Fainting
-
Uncomfortable rapid heartbeat
Other symptoms are:
-
Brain fog
-
Fatigue
-
Headaches
-
Blurry vision
-
Tremor
-
Nausea
Did you know?
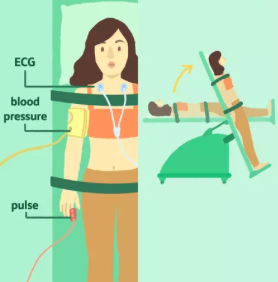
The most common way to diagnose POTs is by conducting a Tilt-Table Test. This test measures the heart rate and blood pressure of the patient when changing posture and position.
DIAGNOSIS
Tilt-Table Tests
-
The most common way to diagnose POTs is by conducting a Tilt-Table Test. This test measures the heart rate and blood pressure of the patient when changing posture and position.
Other
-
Blood or Urine tests
-
QSART-measuring autonomic nerves that control sweating
-
Autonomic breathing test to measure blood rate and pressure response during exercise
-
Tuberculosis skin test
-
Skin nerve biopsy
-
Echocardiogram
-
Blood volume with hemodynamic studies
CAUSES
According to Johns Hopkins Medicine, the causes of POTS are still not fully determined, however, one thing that researchers have noted is that it is more common in women than in men and that adolescents and young adults are more prone to developing the condition. Although the cause of the condition may be unknown sometimes, some recognized causes of the condition are the following:
- alcohol or metal poisoning
- alcoholism
- chemotherapy
- genetics
- genetically inheriting trait of too much noradrenaline
- hypermobile Ehlers-Danlos syndrome
- reduced blood volume
- other underlying conditions associated with secondary POTS (cancer, diabetes, lupus, amyloidosis, Sjögren’s syndrome, and sarcoidosis)
Additionally, POTS may develop spontaneously after a serious bodily stressing event such as after a pregnancy, traumatic event, or viral illness. It is also common for it to develop or appear along with chronic fatigue syndrome. Patients who have peripheral nerve damage and a family history of POTS may develop a higher risk to the condition.
Causes of Types of POTS:
- Neuropathic POTS – This type of POTS is linked with damage to the small fiber nerves. Small fiber nerves are the nerves that regulate the constriction of the blood vessels in the arms, legs and abdomen.
- Hyperadrenergic POTS – Hyperadrenergic POTS is a type of POTS that is caused by higher than usual levels of a stress hormone known as norepinephrine. Norepinephrine can act as a stress hormone, however, it is also a neurotransmitter which means that the brain’s perception of stress can play a larger role than the actual stressor.
- Hypovolemic POTS – A type of POTS linked to abnormally reduced levels of blood plasma levels (hypovolemia).
- Secondary POTS – A type of POTS that is associated with another condition that can cause autonomic neuropathy (i.e., diabetes, Lyme disease, and autoimmune disorders such as lupus)
- Autonomic neuropathy, or dysautonomia, is a dysfunction of the nerves responsible for controlling unconscious bodily functions such as heart rate, blood pressure, digestion, and water retention/reduction.
SOLUTIONS
TRADITIONAL SOLUTIONS
PRESCRIPTION
-
There are also a few existing prescription medications that can be used to treat the symptoms of POTS. If you suspect you have POTS or suffer from symptoms of POTS, ask your doctor about these medications. Beta blockers are a class of medication commonly prescribed after a heart attack and used to decrease blood pressure commonly prescribed to people with POTS. Midodrine, a blood pressure medication, is often prescribed to POTS patients to increase pressure. Depending on how POTS affects the individual's blood pressure, one of the previous could possibly be an effective option for blood pressure control in people with POTS. Pyridostigmine is a muscle strengthener often prescribed to POTS patients to manage symptoms of muscle cramps and weakness. Similar to salt tablets, Fludrocortisone is a steroid that increases sodium in the body by decreasing sodium in urine. Another medication, Ivabradine, has been used on POTS patients though it is primarily prescribed for heart failure. Ivabradine increases heart rate without increasing or decreasing blood pressure, though it is very expensive and commonly causes many side effects.
ALTERNATE SOLUTIONS
Ayurvedic
-
Ayurvedic medicine, commonly known as ayurveda, is a multi-thousand year old form of holistic medicine and wellness originating in India. There are very few ayurvedic treatments that have actually been discovered to alleviate symptoms of POTS. Brahmi capsules, which contain the brahmi herb, are known for their ability to clear brain fog caused by POTS and reduce blood pressure. Amla (Indian gooseberry), Ashwagandha (Indian ginseng), and raw garlic can also be used to lower blood pressure for individuals who experience an increase in blood pressure when standing (note: some may experience a decrease in blood pressure). Cardamom and celery juice can be used as ayurvedic anti inflammatories. Celery Juice contains high levels of naturally occurring nitrates which helps reduce blood pressure in addition to being rich in vitamins and minerals, some which are antioxidants. In addition to ingesting natural herbs and medicines, many lifestyle and dietary changes can be made to lessen the symptoms of POTS without taking over-the-counter or prescription medication (see dietary and lifestyle changes).
Over-the-counter
-
Due to the lack of FDA approved drugs and therapies, there are few medications available to treat the symptoms of POTS. These medications and remedies are meant to alleviate the symptoms caused by POTS- not to “cure” the syndrome, as no cure has been discovered. Although they can be purchased over the counter, it is advised that these medications are not taken without a doctor’s recommendation. Note that all medications have side effects. Salt tablets can be taken to increase sodium in the body. An increase in sodium levels causes more blood to circulate, therefore increasing blood pressure and lowering heart rate. Other over the counter treatments also include any blood pressure support supplements.
Nutrition
-
In order to reduce the symptoms of POTS, there are specific nutritional and diet recommendations. It is recommended to drink 2-2.5 liters (64-80 oz) of water daily along with small and frequent meals. Importantly, adding extra salt (extra 3-10 g per day) to one’s diet increases circulatory blood volume and therefore lowers heart rate and increases blood pressure. Increasing blood pressure and lowering heart rate reduces the symptoms of POTS. Beneficial high-salt foods include broths (vegetable or meat), pickles, olives, salted fish, and nuts. Additionally, consuming adequate amounts of soluble fiber and complex carbohydrates can help reduce blood sugar spikes which can reduce POTS symptoms. It is best to avoid processed foods because they have lower nutritional value and contribute to POTS symptoms such as fatigue. Overall, nutrition should be balanced with a variety of proteins, vegetables, dairy, and fruits.
LIFE-STYLE CHANGES
How can you deal with POTS in everyday life?
Positions for When Experiencing an Episode
- If possible, lie down with your legs raised over your head level OR
- Cross your legs while in a standing position, rock back and forth on your feet, and/or clench your buttocks, stomach muscles, or fists
- Both these methods attempt to counter a decrease in blood flow that occurs with POTS
Find a routine healthcare provider
Meditate, mindfulness, and taking care of your mental health
Bad mental health, stress, and anxiety have all been proven to affect the symptoms and severeness of POTS. Stress and anxiety have impacts on blood pressure and heart rate that can cause permanent changes to physiological function when these mental states are overexpressed. Since those diagnosed with POTS (specifically hyperadrenergic POTS) can be more sensitive to norepinephrine, which is released by our bodies when anxious or stressed, taking care of this is very important. Practices such as mindfulness, meditation, and therapy can all have positive effects on your mental health and therefore may also help lessen any POTS symptoms.
Prepare for waves of fatigue by
- Prepare easy-to-make or reheat meals for times of fatigue to ensure you maintain healthy eating patterns. By establishing a routine for meals you can prevent spikes/crashes in blood sugar levels which can heighten many POTS symptoms temporarily.
- Plan activities where you are actively moving around (such as showering, driving, making errands, etc.) with rest time in between to avoid overstraining your body.
- Start using stools, shower chairs, wheelchairs, etc. to make your daily routine less strenuous
Start writing a health journal
- Take note of daily blood pressure with a blood pressure monitor at home
- when blood pressure is 140 over 85 or higher, a POTS specialist or other healthcare provider should be informed
- Keep note of any notable symptoms and side effects
- Write down any changes in symptoms or effects
- Make notes and questions for doctors
Compression Stockings
Compression stockings can increase the blood flow back to the heart when worn on the lower body. Compression garments such as stockings and leggings are recommended to those diagnosed with POTS.
Sleep Schedule
Maintaining a consistent sleep pattern, waking up and going to bed at around the same time each morning and night, helps the body achieve a more consistent and stable rhythm in the long term. The recommended sleep time per night is 7-10 hours.
Exercise
Exercise can improve your overall health and having a healthier body can help alleviate and lessen all types of POTS symptoms. However, strenuous activities are also very difficult for POTS patients, so one recommended type of exercise is isometric exercise. Isometric exercise is the squeezing and contraction of muscles in the body with little movement. It can be done in a sitting or lying down position. One recommended isometric exercise program to follow is
COVID-19 IMPACT
-
POTS PATIENTS:
As the COVID-19 pandemic progresses through time, researchers are learning more and more about the potential long term implications of contracting the virus, and the types of complications these so-called “COVID long-haulers” are facing. One such complication being studied is post-COVID POTS. Some researchers believe that the coronavirus can potentially trigger POTS, with an increasing number of individuals who contracted and recovered from the COVID-19 virus experiencing POTS-like symptoms. These symptoms include increased heart rate, brain fog, tachycardia, and severe chronic fatigue. People who have experienced these POTS-like symptoms have ranged from having mild cases of COVID-19, to more severe cases. However, the Johns Hopkins Division of Infectious Disease has observed that the majority of patients with post COVID-19 POTS seemed to have had rather mild cases of COVID-19 often times being asymptomatic (asymptomatic pertains to an individual who did not show any symptoms that are normally associated with a COVID-19 infection while infected). If you have previously contracted COVID-19 and are experiencing the following symptoms, consider discussing these problems with your doctor, as this may be an indication of post-COVID POTS.
OTHER COVID FACTS
- The COVID-19 virus may possibly trigger POTS as the virus targets and affects the autonomic nervous system.
- Some individuals who are suffering from POTS after having a COVID-19 infection are developing POTS symptoms during the acute phase (infectious) of their COVID-19 infection, while other patients don’t see their POTS symptoms until a couple weeks after the acute phase of their infection.
- POTS can be triggered by many other types of infections, surgeries, pregnancy, or concussions.
- In a research study done to examine 20 patients who presented with POTS symptoms after COVID-19, 85 percent of the participants reported improved conditions following both drug therapy (medication), as well as non-pharmacologic therapy (therapy without the use of drugs).